enriched claim status.
Is manual claim follow-up consuming too much of your billing team’s time? Instead of manually checking the status of every claim across all your different payers, embrace the future of claims management with Enriched Claim Status from Janus Health. Our intelligent automation saves time and money by eliminating the need to manually check claim status in different payer portals.
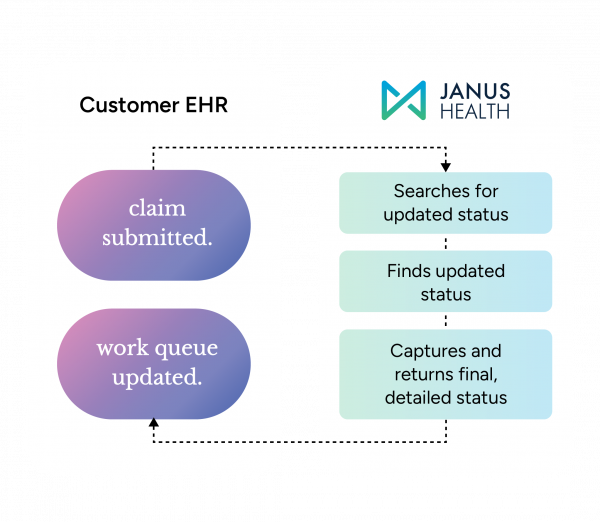
Enriched Claim Status automatically sends a detailed claim notification to the electronic health record (EHR) when a change in claim status occurs, so team members have the information they need at their fingertips. This enables them to more immediately focus their attention on the claims that need additional information to be processed and paid, resulting in quicker payment.

proven results.
Our cutting-edge claim status optimization results in less administrative work and quicker payment for your healthcare organization. When your team implements Enriched Claim Status to streamline their workflows, you can save an estimated 12% in labor overhead for insurance follow-ups.
Memorial Healthcare System replaced an older vendor and is now checking the status of 4,000 claims daily, a time savings of 5 hours per day.
how enriched claim status works:
Our cutting-edge technology is a game-changer when it comes to claims management. When the status of a claim changes, all the relevant information is sent to your EHR. We know what details are important, so we provide:
- CARC and RARC codes
- Denial comment where available
- Line-level payment detail where relevant
- Check number
- Patient responsibility
If the status remains pending, Janus Health tracks the progression of the claim and escalates it so it can be resolved in a timely manner.
Backend Automation
Timely, Detailed Status Updates in Your EHR
Detailed status information, including a portal screenshot, is sent directly to the EHR when there is a claim status change. Our technology ensures your team has the most up-to-date claims information, and there’s no need for them to manually check accounts with no updates.
Act Only When Needed
Enriched Claim Status empowers your team to focus only on the accounts that truly require attention. A claim notification with Janus Health’s proprietary task grouping is sent to the EHR when a payer requests action or more information about a claim. This seamless process keeps the workflow optimized and the team operating at peak efficiency.
Even Better With Teleport.
Pairing Enriched Claim Status with our Teleport intelligent automation gives your accounts receivable team one-click payer portal account access from within your EHR. Adding Teleport can shave even more time off your administrative overhead, removing the hassle of logging in and out of payer portals.
seamless integration with existing technology.
We understand how critical it is for our customers to leverage our solutions with their existing systems and technology. That’s why we’ve mindfully built intelligent automations that allow for the smooth and efficient exchange of data. This includes pertinent details from all in-scope payers, offering a complete and consolidated view to facilitate streamlined operations.
Janus Health is committed to seamlessly integrating claim status information into your workflow by delivering comprehensive data through a 277 EDI message. To be compatible with Enriched Claim Status, your EHR must also be capable of generating an 837 file for claim submission and an open account balance flat file.
boost revenue with streamlined claims management.
Is your team spending more time than ever on manual claim status inquiries? Discover how Enriched Claim Status can automate mundane tasks and transform your revenue cycle with a more efficient and engaged team.

